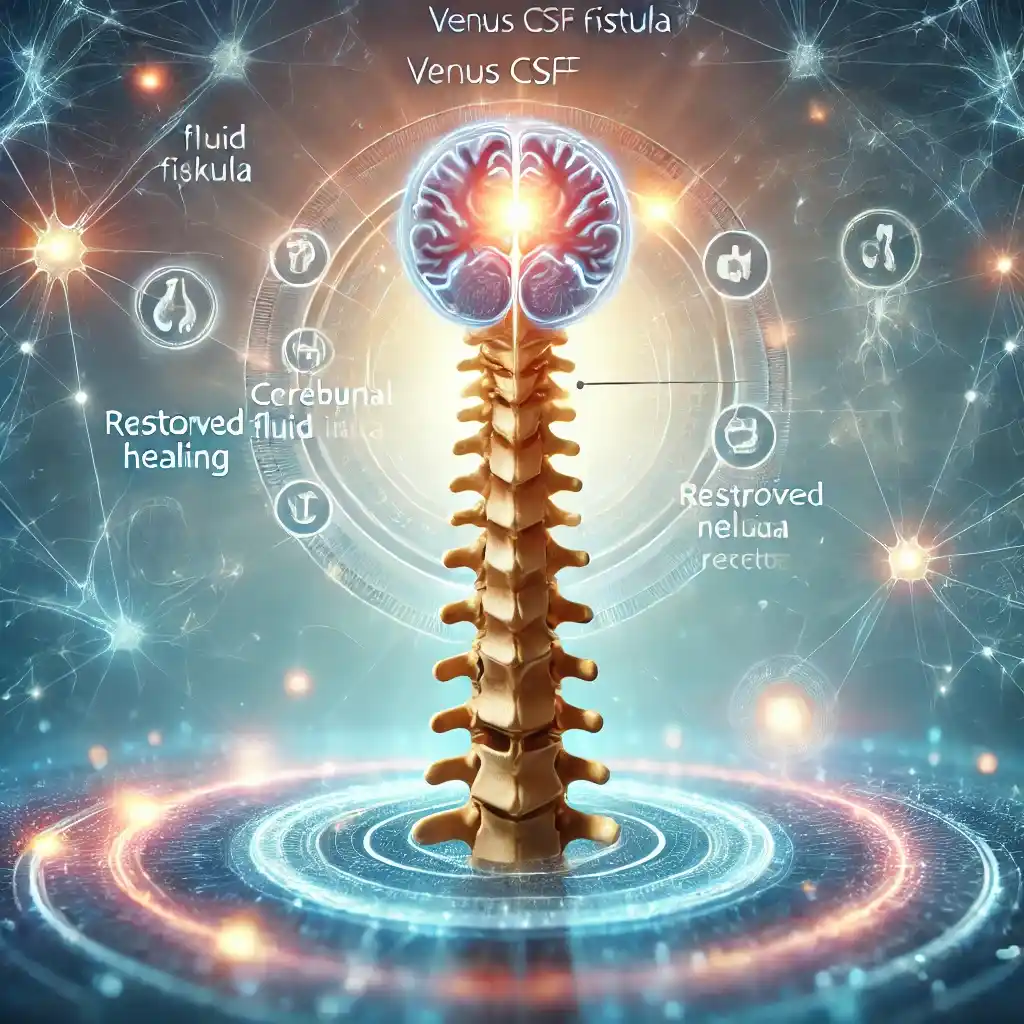
Overview
CVFs are abnormal connections between the spinal subarachnoid space and adjacent paraspinal veins that allow unregulated egress of CSF into the venous system. Resultant CSF depletion causes intracranial hypotension. Although this entity was first recognized very recently, it has rapidly emerged as a very common cause of underlying spinal CSF leak in SIH, particularly in the challenging population of patients with no leak seen on initial spinal imaging.